Software has changed many aspects of our lives, and perhaps nowhere more so than healthcare, a heavily regulated industry with complex data requirements. With technology being a major influencing factor, integrating technology with medicine is quickly modifying how it works. From personalized medicine to telehealth and artificial intelligence, as well as mobile health apps, every such facet is important in setting this new era of healthcare.
Personalized medicine is one of the largest areas impacted by software evolution. Medicine was traditionally practiced in generalizing treatment protocols. Treatment might not be appropriate for all patients at times. As we see more and more sophisticated algorithms alongside the plethora of data analytics tools, healthcare slowly makes its way to personalized medicine. These tools can handle huge data volumes on patients from genes through lifestyle habits and environmental impact to establish a personalized treatment plan.
For example, next-generation sequencing has become extremely cheap and accessible to more people, leading the genetic underpinnings of a wide array of disorders to be extensively studied. This is followed by analyzing the genomic data with software tools that find certain mutations and project how a patient might respond to different treatments. This has the potential to enable healthcare providers to create treatment plans that are significantly tailored and, in turn, potent considering their usage and less likely to produce adverse reactions. Finally, predictive analytics can be utilized to model disease risks, allowing for early interventions and personalized preventive strategies unique to each patient.
Another revolutionary change that software has made possible relates to telemedicine and remote monitoring. In recent years, the importance of telehealth platforms has risen drastically, especially considering how events around the world have increased the demand for innovative solutions in remote care. It allows patients to consult healthcare personnel and professionals using video calls, which reduces the need for physical visits in hospitals seeking healthcare services, hence increasing access to healthcare. It is a significant milestone, especially for chronically ill patients who need follow-up and consultation services at regular intervals and may not have the opportunity to travel as often.
Wearable devices and home health monitoring systems… are key players in the management of chronic conditions. All are devices that monitor vitals, activity, and other health measures remotely in real-time to healthcare delivery mechanisms. This near-continuous stream of data at hand makes it possible to monitor the patient’s health more continuously and enables timely intervention as well as changes in treatment. All of this will enable patients to engage more with their health management, thus ensuring improved adherence and outcomes for the treatment regime.
Another characteristic innovation, electronic health records, has also led to seismic alterations in the health care supply. Digital formats: EHR systems are the digitized version of paper records, as they are unlike physical or computer files, excel sheets, and databases. Current EHRs offer a comprehensive view of patient history or information, giving laboratory results and a treatment plan for the past consultation. The data integration of this type improves workflow, reduces errors, and reduces communications overlap between the providers.
They also require analytics tools that can identify trends and patterns in patient data. It helps with evidence-based decision-making since you get a sense of how well the treatment works, what happens to the patient, and where deficiencies can be redressed if any. These data are thus useful to healthcare providers, who can use them for better decision-making and adjust therapies according to individual requirements.
images X-rays, MRIs, and CT scans with impressive attention to detail. Algorithms detect abnormalities like tumors or fractures. AI helps in faster diagnosing, as it works fast and superbly on complex imaging data to get better accuracy, thus identifying more severe cases.
This is then enhanced with AI (artificially intelligent) machine learning models that apply more sophisticated algorithms to large datasets to make predictions about epidemics, health outcomes, and treatment responses. These models discover unseen patterns and correlations that would not be visibly available to a clinician by directly visualizing the data. For example, a predictive model can predict if a patient would suffer from a particular disease by analyzing the medical record data along with genetic information and demographic details. It will also enable early interventions and hence personalized strategies to help in attaining improved clinical outcomes for the patients as well as optimizing resource utilization.
Decision support systems stem from another major change in the software landscape. They deliver real-time, evidence-based recommendations and alerts that help support clinicians. Clinical decision-support systems (CDSS) are organizations that have planned principles governing the management of plans for patients founded upon individual profiles. This reduces the cognitive burden on healthcare providers and reduces errors to ensure that care decisions align with clinical best practices.
In addition, interaction checkers built into the EHR or stand-alone applications will screen drug lists for possible interactions, which introduces another level of safety. Tools like these can and do prevent adverse drug reactions to make sure that the patient is treated safely and effectively.
This in turn sped the improvement of medical research and uncovering drugs thanks to faster-draining software. This has altered the way research is performed by enabling researchers to rapidly identify prospective drug candidates and accelerate the onset of clinical trials because we can handle so much data. Here, simulation and modeling tools for enabling scientists to simulate biological processes and drug interactions help by offering lessons learned before the costly stage of clinical trials. In this way, the research pipeline is smoothed to develop new therapies faster and make innovative treatments get into our market sooner.
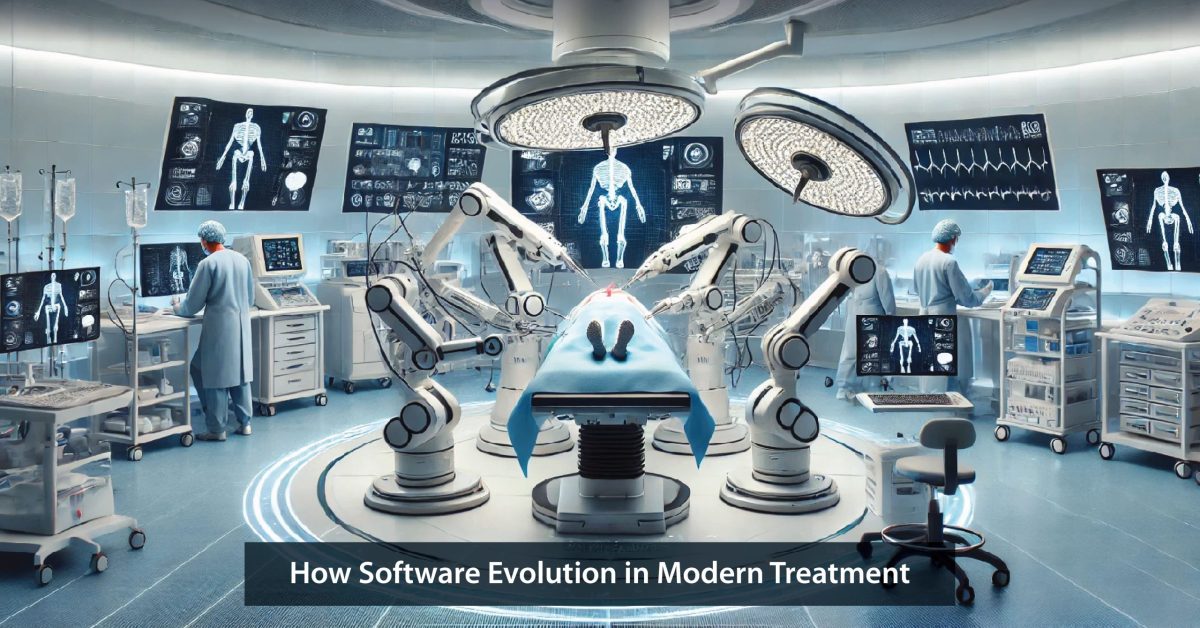
This would also be a giant step in medical technology, robotic surgery, and automation. This highly sophisticated software offers surgical precision and is associated with minimally invasive surgery techniques. When combined with direct surgeon input and enhanced by sophisticated software, precisely controlled robots enable surgeons to perform complicated procedures via a more minimally invasive technique, leading to quicker recovery times. Automated laboratory tests and image analysis are efficient, precise ways to reduce the likelihood of error by human intervention as well as expediting diagnosis.
Over the expansion of mHealth applications, patients have been able to manage their health in ways they never could before. It includes smartphones and other apps that monitor exercise, diet, sleep patterns, and mental health. mHealth applications encourage behavior change by providing real-time feedback and sending tailored messages that suggest reminding patients to adhere more completely to their treatment plans or engage in better preventive care. It adds a healthy dimension to your life by making you involved in accountability and goal setting along with progress tracking through interaction from the health provider’s end, thereby following more teamwork towards managing health.